Methods of Hemostasis
The surgical team can stop bleeding and achieve hemostasis in three unique ways, click on the boxes to learn more:
Mechanical
- Direct pressure such as holding a sponge or towel on a bleeding site
- Suture materials
- Ligating clips
Thermal-Based Energy
- Electrocautery
- Lasers
Chemical
- Medications
Let us look at each of these methods more closely.
Methods of Hemostasis – Mechanical
Different mechanical tools can be used during surgery to provide temporary or permanent hemostasis.
(Phillips & Hornacky, 2020)
📁 Documentation Highlight
Clips used for hemostasis must be meticulously documented in the patient record because it is vital to keep track of any implants being left in the patient. Why is this important? If the patient requires any diagnostic imaging in the future, including an MRI, the technicians need to be able to identify if there are metal implants and if they are MRI-compatible. Follow your institution’s charting policies as to what is required for documentation.
Thermal-based Energy
Different thermal-based equipment can be used during surgery to provide hemostasis.
(Phillips & Hornacky, 2020)
Chemical Methods
Chemical methods of hemostasis work to react with blood to form a clot. Many of these chemical materials will re-absorb over time as the body heals. They do not have to be removed. There is one exception. Hemostatic chemical materials cannot be packed into a closed space where they could swell and cause pressure on surrounding tissues such as the spinal canal, or in neurosurgery. In this instance, surgeons will still use a chemical agent but will carefully ensure it is removed before closing.
Click on the various chemical hemostatic agents below to learn more about them. There are many quick videos to provide you with a visual and overview of the agent from their supplier. It is vital that perioperative nurses are knowledgeable about and follow the manufacturer’s directions for hemostatic agents, sealants, and adhesives.
(ORNAC, 2021)
Absorbable Gelatin (Gelfoam)
- It can come in a powder or foam pad.
- It is an absorbable hemostatic agent.
- It can be cut without crumbling.
- When placed on a bleeding capillary, it swells and forms a large clot.
- It may be soaked in a liquid such as saline, thrombin, or epinephrine, depending on the surgeon’s preference.
Oxidized Cellulose (Surgicel)
- It can be cut into strips and laid directly on a bleeding or oozing site.
- When oxidized, cellulose forms a clot quickly as soon as it touches blood.
- It is good to use in areas where it is difficult to control bleeding by other methods.
- It is not recommended for use on bone as it can inhibit bone regeneration unless it is removed before closing the wound.
Oxytocin
- Oxytocin may be directly injected into the uterine muscle to cause a contraction during c-section surgery.
- It can be injected systemically to help with a hemorrhage from the uterus.
Epinephrine
- Epinephrine is a vasoconstrictor.
- It can be used topically within an incision on gelfoam sponges. It is commonly used in ear and microsurgical procedures.
- Epinephrine can be absorbed systematically and can cause cardiac stimulation. Care must be taken when using epinephrine. It is often diluted and only used in lesser amounts.
Silver nitrate
- Silver nitrate comes in the form of applicator sticks. These are applied topically to cause vasoconstriction.
- It is commonly used in burns or on nasal and oral surgical sites.
- It can help seal areas that cannot be surgically closed and must be left to heal by secondary intention.
Thrombin (Tisseel, Floseal)
- This accelerates the coagulation of the blood and helps with capillary bleeding. It combines with fibrinogen to form a clot.
- Thrombin can come as a powder that is sprinkled on a wound.
- Hemostatic devices such as Tisseel and Floseal combine Thrombin with other active ingredients to achieve hemostasis.
- This accelerates the coagulation of the blood and helps with capillary bleeding. It combines with fibrinogen to form a clot.
- Thrombin can come as a powder that is sprinkled on a wound.
- Hemostatic devices such as Tisseel and Floseal combine Thrombin with other active ingredients to achieve hemostasis.
Collagen (Surgiflo, Hemopatch)
- Collagen is an absorbable, topical hemostatic agent.
- It is applied dry.
- There is an adhesion of platelets when it meets a bleeding surface, and fibrin is deposited within the collagen.
- It must be applied with firm pressure against the bleeding surface.
(Phillips & Hornacky, 2020)
🧠 Graded Activity
In Blackboard complete the Graded Activity: Methods of Hemostasis.
💬 Communication Highlight
While the surgical team works to obtain hemostasis and control bleeding, it is not always enough. The perioperative team must communicate and work together to recognize when there is substantial blood loss. The scrub nurse must keep track of the amount of irrigation fluid used during a procedure so that this can be considered when reviewing the amount of blood/fluid in the suction canisters and saturated sponges. The team estimates the total blood loss and through analysis of blood work, determines if a transfusion of blood product is required.
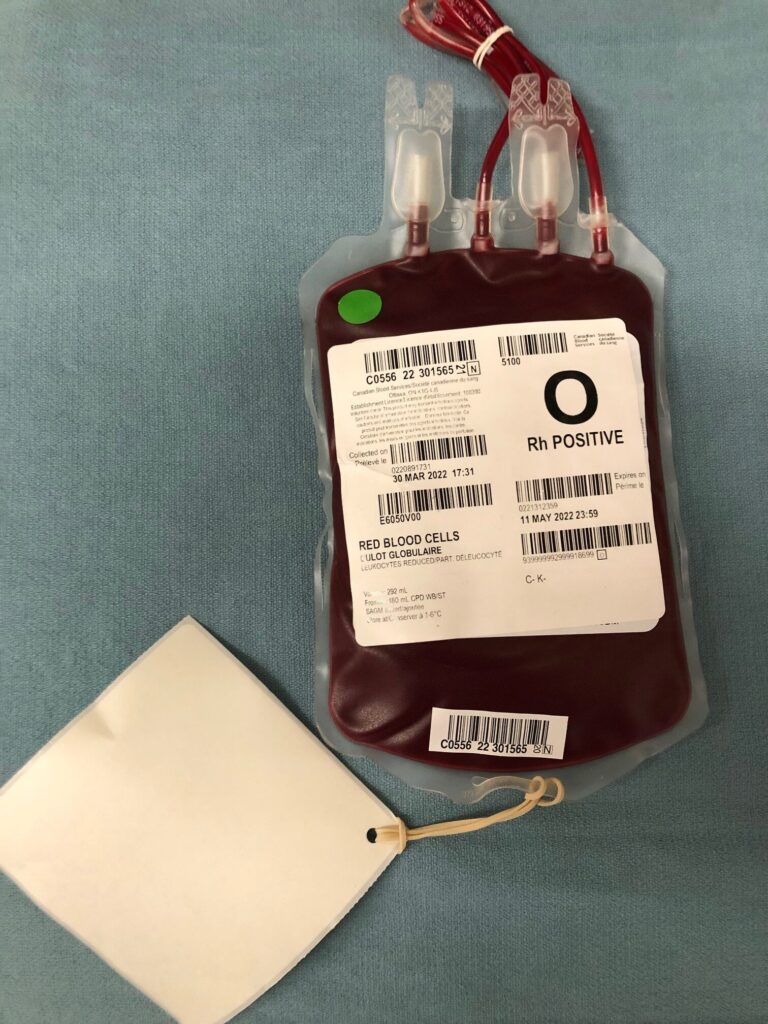
When Blood is Needed During Surgery
Despite the surgical team’s best efforts to obtain hemostasis, there may be a need to transfuse a patient. Depending on the surgical procedure being performed and the risk for blood loss, the patient should be typed and crossed out before their procedure and a blood transfusion consent should be signed.
Screening before surgery
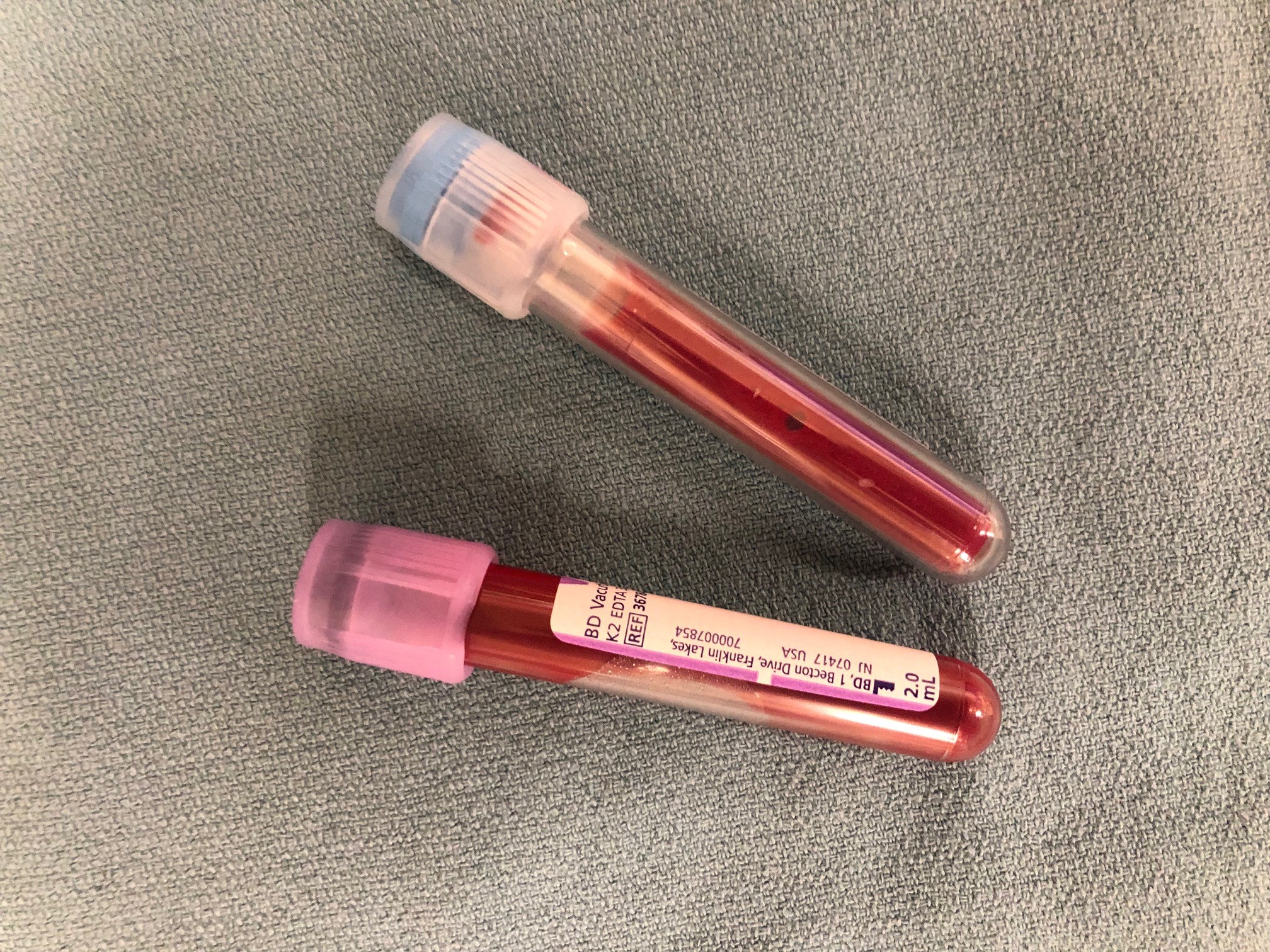
Group and Screen
A group and screen allow the blood bank to:
- Determine the patient’s blood group: ABO (0, A, B, AB)
- Rh(D) which can be negative or positive
- It also allows the blood bank to test for antibodies in the patient’s plasma.
- If the patient does have antibodies (positive) they may experience hemolysis if they are transfused with the corresponding antigen positive Red Blood Cell.
- In these cases, the blood bank will do further testing to identify the antibodies; for example, anti-D, anti C, anti-K.
Crossmatch
- The results of the group and screen can then be used to cross-match the red blood cells (RBCs) to ensure they are compatible for transfusion.
- The blood sample used to crossmatch a unit of blood can only be used for 96 hours (about four days) after the first unit of blood is transfused. This is to ensure that no new antibodies have been produced.
- For more information, download the following document: Bloody Easy: Blood Administration Version 3.
In some cases, the surgical team may not anticipate a need for blood transfusion, or the patient may come into the OR urgently before a proper type and screen or crossmatch can be completed. In these situations, perioperative nurses must follow the hospital protocol for requesting uncross matched blood.
Then the blood bank will issue Group O Rh(D) negative RBCs for females of childbearing age. It will issue Group O Rh(D) positive for all male patients, and for female patients past childbearing age.
The patient will receive Group O blood ONLY until the patient’s ABO group and Rh(D) screen can be completed.
(Berta, 2021)